If I Only Knew
- Who decides what things are worth doing?
- Do we possess knowledge of disease or a proxy of knowledge?
- Are we trapped by the historically successful paradigm of Virchow et al?
- How do we best transfer knowledge to learners?
- Why do we not have graded responsibility in pathology residency training?
- What is the best way to teach risk management in surgical pathology?
- What are the risks and benefits of communicating uncertainty in pathological diagnosis?
- Is reductionism a dead end?
- Should we have informed consent in surgical pathology?
- How do we maximize group intelligence?
I hope it is not pedantic for me to claim that I could expand on each of these questions. My children know I love to lecture! I had to leave out a longer list of important questions including the critical role of anatomical location in human disease, currently completely unknown1. But I think I will choose questions 1, 2, and 3. I love to rant about these.
1. Who decides what things are worth doing?
“A job not worth doing is not worth doing well.” I hope this adage makes it past the censors, it may be too cynical for a profession of caregivers. This advice was actually given to me in my first year of practice! The adage is, of course, the inversion of the better-known bromide: “A job worth doing is a job worth doing well.” This older version is also important, but its inversion offers a practical strategy for coping with professional absurdity.
Let me give you an example. In head and neck pathology, we are sometimes asked to count the number of eosinophils per HPF in sinus mucosal biopsies. We are told that if this number is over 10 that it impacts patient management. I have no doubt there is a paper in the literature justifying this treatment algorithm. But does anyone actually think that a patient with 9 eos per HPF should be treated differently than someone with 11 per HPF? We find comfort in quantification because it seems better than “gestalt” judgments (for example, “there are a lot of eos”). But as our practices pursue this sort of measurement minutia, do we overburden ourselves with labour of dubious merit, and at the same time offer up a false promise of mathematical pathology?
2. Do we possess knowledge of disease or a proxy of knowledge?
Do we possess true knowledge? That’s a tough one, alright. Modern diagnostic pathology is not the study of disease, but the classification of disease: nosology. The Royal College (RCPSC) wants to rename our specialty and although I’ve always told Mike Nimmo that my suggestion was going to be the “Department of Pathology and Margin Assessment” perhaps we should be called nosologists instead. I’ve long been fascinated by the modern controversies pertaining to cladistics (in this sense: the relationships between diseases). Some of you may not know that there is a vibrant debate in microbiology about the reordering of fungal species based on genomic data. Here’s a quote from a large consensus statement:
“Should the proposals be accepted, the meaning of nomenclatural types would change in a fundamental way from physical objects as sources of data to the data themselves. Such changes are conducive to irreproducible science, the potential typification on artefactual data, and massive creation of names with low information content, ultimately causing nomenclatural instability and unnecessary work for future researchers that would stall future explorations of fungal diversity.”
I know there’s a lot to unpack there. I reference the very interesting consensus statement below2, but I will summarize it here to say that fully incorporating molecular information could destabilize our categorization of disease. Maybe that’s a good thing. Maybe it isn’t. But at least microbiologists are dealing with the question.
It all gets back to what we regard as knowledge. Richard Feynman has offered an interesting personal anecdote about his childhood (available on YouTube) where his father explains to him around the age of 5 that naming something does not mean you understand it. It’s certainly a first step, as Linnaeus showed us, but only that. Barely that.
3. Are we trapped by the historically successful paradigm of Virchow et al?
Are we trapped in success? Let me suggest to you that the history of knowledge acquisition in microscopic pathology, like pretty much everything, follows a sigmoid curve.
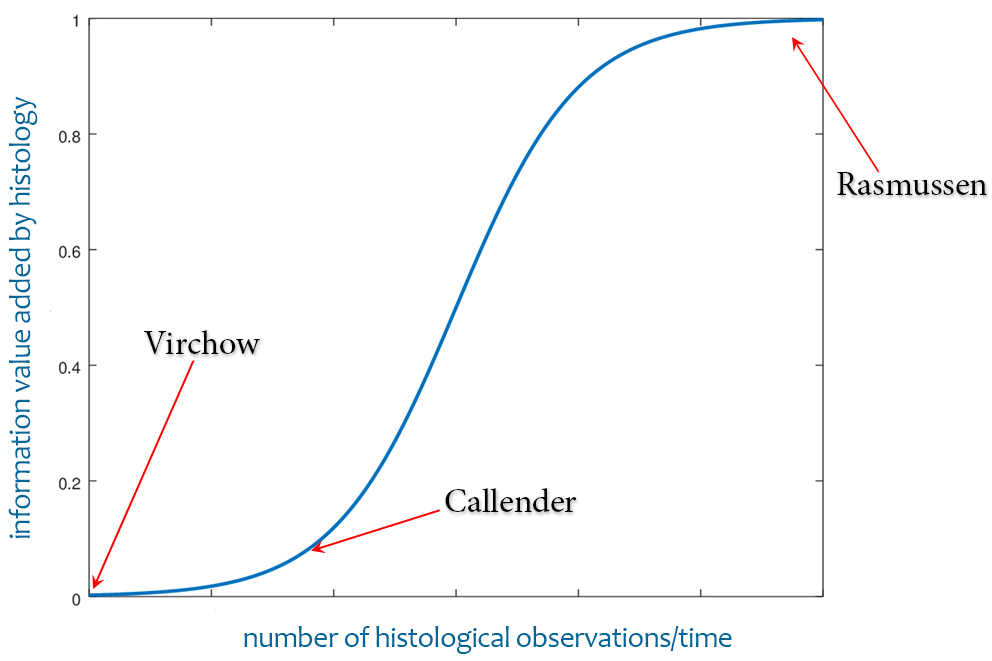
When Virchow added microscopic assessment to pathology, he introduced a whole new tool to pathology with the potential for future investigators to add massive data sets to our understanding of disease. George Russell Callender was an early adopter. In the 1930s, he established that there were different “kinds” of uveal melanoma. Astute physicians like Osler could easily see that pathology was on the rise and there was no telling how high it could go. Everyone wanted a piece of pathology.
Now, after 150 years those massive data sets have been duly added, but the curve is flattening. Now it is necessary to add more and more microscopic observations to achieve very marginal increases in value (value regarding the knowledge of human disease). You can see where I am on the curve, and it is not an easy spot to be in!
One more thing.
There is currently a debate in head and neck pathology about what to call unconventional forms of squamous dysplasia. These are diseases that act like dysplasia but don’t look like it. Much progress in this domain was initiated and advanced by members of our department like Drs Gilks and Hoang who understood that cases of vulvar intraepithelial neoplasia didn’t always read the textbooks.c
But regarding the debate in head and neck circles, I don’t get it. They want to rename these diseases (proliferative verrucous leucoplakia, verrucous hyperplasia, keratosis of uncertain significance, etc etc). The experts say we can’t call these lesions dysplasia because they don’t look like dysplasia. But they are dysplasia (disordered neoplastic growth)! The pathology experts are mistaking their knowledge of microscopic morphology for “the thing in itself” (Kant). They are confusing their proxy of knowledge for the actual disease process. At the very least, they are misapprehending the truth content of names.
Spinoza said (something like) “what is knowable is simply the contents of our awareness.” Maybe that sounds like an impractical caveat to practicing pathologists, but it would be good for us to continually reaffirm the limitations of knowledge and the way in which bias shapes our interpretations. Human language is a system of symbols that categorizes ideas to enable communication. Pathology is a system of names that attempts to reduce an almost infinite number of diseases to a more or less manageable list, thus facilitating study. But these systems are arbitrary and have many constraints. I have been able to practice pathology without really understanding it. I hope that new minds can make better progress, and I wish them good luck in the journey.
But please don’t get me wrong. My own travels have been abetted on all sides by wonderful colleagues. It is impossible for me to imagine a better profession, or people I would have rather worked with all these many years. We look down microscopes at patterns, and then we turn to each other and talk. It is a marvel.

